Publications
Dysfunctional neuro-muscular1 mechanisms explain gradual gait2 changes in prodromal spastic3 paraplegia
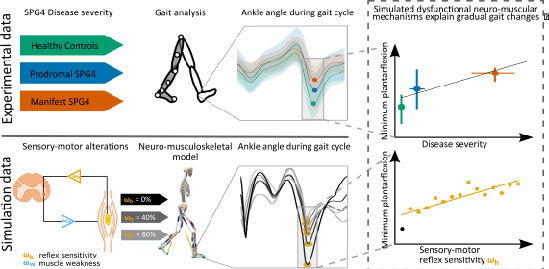
In Hereditary Spastic Paraplegia (HSP) type 4 (SPG4) a length-dependent axonal degeneration in the cortico-spinal tract leads to progressing symptoms of hyperreflexia, muscle weakness, and spasticity of lower extremities. Even before the manifestation of spastic gait, in the prodromal phase, axonal degeneration leads to subtle gait changes. These gait changes – depicted by digital gait recording – are related to disease severity in prodromal and early-to-moderate manifest SPG4 subjects. We hypothesize that dysfunctional neuro-muscular mechanisms such as hyperreflexia and muscle weakness explain these disease severity-related gait changes of prodromal and early-to-moderate manifest SPG4 subjects. We test our hypothesis in computer simulation with a neuro-muscular model of human walking. We introduce neuro-muscular dysfunction by gradually increasing sensory-motor reflex sensitivity based on increased velocity feedback and gradually increasing muscle weakness by reducing maximum isometric force. By increasing hyperreflexia of plantarflexor and dorsiflexor muscles, we found gradual muscular and kinematic changes in neuro-musculoskeletal simulations that are comparable to subtle gait changes found in prodromal SPG4 subjects. Predicting kinematic changes of prodromal and early-to-moderate manifest SPG4 subjects by gradual alterations of sensory-motor reflex sensitivity allows us to link gait as a directly accessible performance marker to emerging neuro-muscular changes for early therapeutic interventions.
Specific gait changes in prodromal hereditary spastic paraplegia type 4 - preSPG4 study
Background: In hereditary spastic paraplegia type 4 (SPG4), subclinical gait changes might occur years before patients realize gait disturbances. The prodromal phase of neurodegenerative disease is of particular interest to halt disease progression by future interventions before impairment has manifested. Objectives: Identification of specific movement abnormalities before manifestation of gait impairment and quantification of disease progression in the prodromal phase. Methods: 70 subjects participated in gait assessment, including 30 prodromal SPAST mutation carriers, 17 patients with mild-to-moderate manifest SPG4, and 23 healthy controls. Gait was assessed by an infrared-camera-based motion capture system to analyze features like range of motion and continuous angle trajectories. Those features were correlated with disease severity as assessed by the Spastic Paraplegia Rating Scale (SPRS) and neurofilament light chain (NfL) as a fluid biomarker indicating neurodegeneration. Results: Compared to healthy controls, we found an altered gait pattern in prodromal mutation carriers during the swing phase in segmental angles of the lower leg (p