Gait in hereditary spastic paraplegia – from axonal degeneration to movement disorder
Research Area:
Clinical Movement Control and real-life Behavior Analysis for Assistive SystemsResearchers:
Christian Laßmann; Winfried Ilg; Jens Seemann;Collaborators:
Tim Rattay (HIH Department of Neurodegeneration); Ludger Schoels (HIH Department of Neurodegeneration); Daniel Häufle (HIH Department Motor Control Modeling)Description:
In Hereditary Spastic Paraplegia (HSP) type 4 (SPG4 / SPAST) a length-dependent axonal degeneration in the cortico-spinal tract leads to progressing symptoms of hyperreflexia, muscle weakness, and spasticity of lower extremities. The therapeutical potential for future intervention is likely most promising in the early stages of HSP. Therefore, it is crucial to identify and quantify first changes already in the prodromal phase of HSP patients.
 |
|
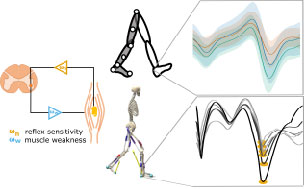
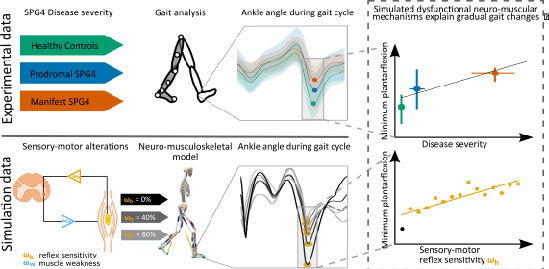
Figure 1 We first used data of an instrumented gait analysis to investigate gait changes of healthy controls (green), prodromal SPG4 (blue), and manifest SPG4 (red) patients. We identified characteristic changes for the three different groups. Secondly, we introduced and gradually manipulated neuro-muscular mechanisms, i.e. hyperreflexia (muscle spindle velocity feedback, orange), muscle weakness (reduced isometric force, light blue), and their combination in a neuro-musculoskeletal model and expected to predict relative gait changes, as in experimental data. |
Specific gait changes in prodromal SPG4 subjects
In order to establish valid performance and biomarkers evaluating treatment responses, we measure gait features that may serve as potential performance markers to quantify gait abnormalities and disease development/progression in manifest and prodromal subjects in a movement laboratory. We found that even before the manifestation of spastic gait, in the prodromal phase, axonal degeneration leads to subtle gait changes. These gait changes depicted by digital gait recording – are related to disease severity in prodromal and early-to-moderate manifest SPG4 subjects1.
Longitudinal gait changes as valid performance markers
We investigate the progressing subtle gait changes in a 10-year longitudinal study with prodromal SPG4 subjects. We analyze disease specific gait changes in the prodromal phase and investigate the multivariate correlations with other biomarkers (e.g., Neurofilament light chain) and clinical scores.
Real-life gait assessment in prodromal and manifest HSP
To establish easily accessible and less controlled motor performance markers, we use multi-variate measures of spastic gait assessed by wearable sensors. Simulations of Dysfunctional neuro-muscular mechanisms explain gradual spastic gait changes. We hypothesize that disease-specific dysfunctional neuro-muscular mechanisms in the prodromal phase of SPG4, such as hyperreflexia and muscle weakness, explain longitudinal and severity-related gait changes2. Therefore, we investigate neuro-muscular dysfunction in a neuro-musculoskeletal model of human walking to reproduce gait changes observed in experimental data3. The gradual alteration of sensory-motor reflex sensitivity to predict kinematic and muscular changes of prodromal SPG4 subjects, allows us to identify neuro-muscular changes and link them to gait as a directly accessible performance marker. These insights may help to design future therapeutic interventions.
Quantifying axonal motor-neuron damage by corticomuscular coherence
To better understand degeneration processes leading to gait changes and impairments in prodromal and manifest SPG4 patients, we investigate electrophysiological methods to quantify axonal damage. The outcome will help us to design more precise neuro-musculoskeletal models to simulate gait changes and axonal damage over time.
